by Danny Levine
Rady Children’s Institute for Genomic Medicine recently completed a two-year pilot project with the state of California that demonstrated its use of rapid whole genome sequencing in real-world hospital neonatal and pediatric intensive care units can not only improve outcomes but also save money.
“There are a lot of critically ill children in the hospital who don’t have a diagnosis, and it’s not clear exactly why they’re sick,” said Lauge Farnaes, assistant medical director for Rady Children’s Institute for Genomic Medicine. “Traditionally whole genome sequencing has been the testing of last resort because it’s relatively expensive. What we wanted to do was show that doing the most comprehensive test upfront to help identify if there’s a genetic cause to why these children are sick is not only the right thing to do in terms of providing better care to the patient, but it’s also the right thing to do economically.”
Rady Children’s has used whole genome sequencing to diagnose babies and children hospitalized in intensive care with rare diseases since July 2016, but only as part of clinical trials. In 2018, the state of California committed $2 million to Project Baby Bear, a pilot project involving five hospital systems in California to see if the use of rapid whole genome sequencing would benefit Medi-Cal infants who were critically ill.
Until the initiation of Project Baby Bear, though, whole genome sequencing was not covered by insurance or Medi-Cal and was available only through clinical trials paid for by research grants or philanthropic donations.
Stephen Kingsmore, president and CEO of Rady Children’s Institute for Genomic Medicine said research studies over the past eight years have consistently shown that children in intensive care units benefit from rapid genome sequencing, but they wanted to show the technology was ready for prime time outside of a research study at multiple sites.
“That was an open question,” he said. “Sure. It’ll work at Rady Children’s where we have a highly trained staff used to using this technology, but what about the real world? That was the question that we set out to answer.”
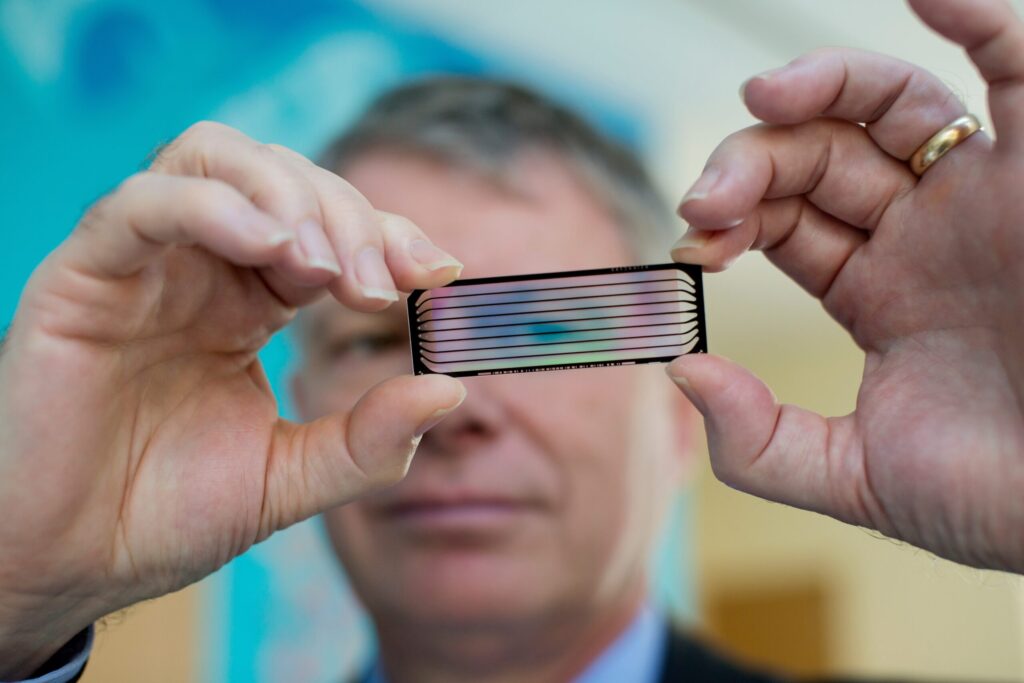
Over the 23 months of the study, the five participating hospital systems completed rapid whole genome sequencing on 178 families and babies. Samples taken from the hospital were sent to Rady, where they were sequenced and analyzed.
The effort provided a diagnosis for 76 babies (43 percent) and led to changing the management of 55 babies (31 percent) that reduced their days in the hospital, and lessened procedures or use of new therapies. The median turnaround time for provisional sequencing results was three days. Some 35 babies who were diagnosed had conditions that occur in less than 1 in a million births, according to a final report on the project.
The use of rapid genome sequencing resulted in 513 fewer days in the hospital, 11 fewer major surgeries, and 16 fewer invasive diagnostic tests. That helped to create overall savings from the pilot study of more than $2.5 million.
As an example of the technology’s power to improve outcomes for patients, Kingsmore pointed to the case of a baby who was born with a slow heartbeat at Orange County Children’s Hospital. The hospital had just begun the program and the doctor ordered the rapid whole genome sequencing and the infant was discharged. Rady sequenced the blood sample and diagnosed the child with Timothy syndrome, a genetic disease that typically leads to sudden infant death syndrome.
“That child’s slow heart rate was not just a benign finding. It actually signaled the fact that she was at high risk of developing a malignant heart disorder that would kill her,” said Kingsmore, who explained they were about to bring the infant back and implant a device that would prevent her from suffering from a life-threatening heart rhythm disorder. “The likelihood that that would have been picked up is zero. It was not on anybody’s differential diagnosis list. In fact, the doctor in charge of the PICU there told us he’d never actually seen it before. They regarded this as basically a lifesaver.”
The pilot test did point to some challenges. Rady said it is important that rather than act like a reference lab that just takes samples and provides results, it needed to act more like a consultative service part of the hospital’s team. Sending an email with a result is not enough. Often a diagnosis was made of a condition the hospital doctors or the physicians at Rady had never heard of. Together they had to figure out the best course of action.
The effort also identified bottlenecks in moving from identifying a patient to getting the result, which needed improvement. One of those is getting doctors to order rapid genome sequencing as early as possible since delays can minimize benefits.
“We want this to be used as what we call a first-tier test. What we mean by that is that it’s part of the initial battery of tests that are ordered on critically ill babies, either on admission or certainly within the first day of admission,” said Kingsmore. “We don’t want this to be a test of last resort, which is offered after all the other test results come back and the doctors go, ‘Okay, let’s get a genome because we’ve done everything else. That’s a mindset change we still need to facilitate for them to bring it to the front of their mind.”
The states of Florida and Michigan are considering instituting similar programs with Rady, which is in discussion with California about the next steps given the program’s success.
Kingsmore said therapeutic development for many rare conditions is stymied by the lack of understanding of how these conditions manifest and progress. Additionally, there is a lack of needed data, such as natural history studies. Access to this data, he said, is a place where RARE-X can help.
“If you don’t know what endpoints to target, if you don’t know the true incidence, if you’re unable to identify affected individuals very early in their disease course, you’re kind of stuck,” he said. “We believe that working through RARE-X, we can solve that and create cohorts of families with rare and ultra-rare diseases, and collect from them the types of natural history information, along with the genome sequences, that enable us to understand the disease to the point where we can pinpoint what it is we’re trying to aim at with novel therapeutic development.”

Stay Connected
Sign up for updates straight to your inbox.
