Diversity of Odysseys: The Diagnostic Challenges of Underserved People with Rare Diseases
The rare disease community is comprised of more than 7,000 individual diseases and represents approximately 400 million people around the world.
For those who have adequate access to healthcare, it takes an average of 7.3 years for a person to get accurately diagnosed after seeing seven or more clinicians.
Many challenges have been previously identified in obtaining an accurate diagnosis including:
- Inadequate insurance coverage of diagnostic testing
- Lack of or no genetic information for a particular disease
- Lack of or no knowledge or awareness of rare disease by clinicians
Delays in diagnosis, or misdiagnosis, can result in devastating outcomes for rare disease families. Historically underserved and/or underrepresented communities can often face additional challenges and barriers to obtaining a proper diagnosis and path to care that need to be identified and addressed through comprehensive and inclusive efforts.
Global Genes is committed to reducing barriers for people with a rare disease who are seeking an accurate and more timely diagnosis. Through this analysis we identified key barriers challenges and obstacles in diagnosing rare diseases, in particular, for underserved communities.
Specifically, this effort aimed to:
-
Better understand the diagnostic landscape for historically underserved and/or underrepresented patients with rare diseases
-
Determine patient and clinical education gaps and resource needs to mitigate barriers and reduce time to diagnosis
Supported by charitable contributions from Travere Therapeutics and Illumina Foundation
Project Overview
To gain a firm understanding of the current diagnostic landscape, effective practices and perceived disruptive barriers for obtaining an accurate and timely diagnosis, we collected data through:
-
Comprehensive literature reviews
-
Analysis of available social media data
-
Individual online surveys with patients, caregivers and clinicians
-
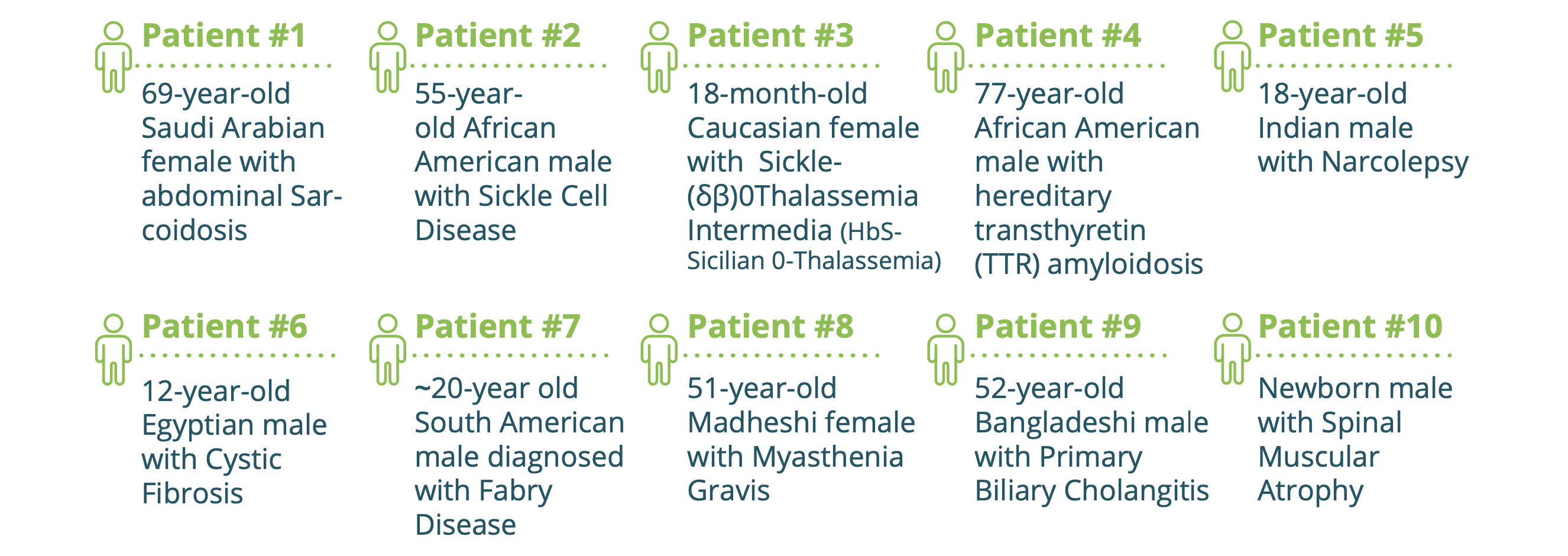
An analysis of 10 rare diseases was also included in order to glean trends and themes regarding diagnostic challenges and barriers across the rare disease landscape.
These diseases included:
• β Thalassemia
• Cystic Fibrosis
• Fabry Disease
• Hereditary Transthyretin (TTR) Amyloidosis
• Myasthenia Gravis
• Narcolepsy
• Primary Biliary Cholangitis
• Sarcoidosis
• Sickle Cell Disease
• Spinal Muscular Atrophy
Case studies for each disease were introduced and described. Relevant social and medical information was reviewed in order to elucidate patient diagnostic journeys and potential differences based on ethnicity or other factors. Case information was derived from primary literature, secondary information and reports, case presentations, and interviews.
Furthermore, patient cases were identified and summarized, leveraging physician narratives in leading journals and publications, as outlined below. Note that this study was limited by the dearth of diverse and representative patient stories in the selected disease areas — identifying another area of need we intend to help address through other initiatives moving forward.
Top Questions Searched for Rare Disease Information
- How is [disease] diagnosed?
- What type of doctor can diagnose [disease]?
- What is the life expectancy of someone with [disease]? • Is there a definitive test for [disease]?
- What is a diagnostic odyssey?
- [Disease] diagnosis criteria
- [Disease] diagnostic test
- What is the treatment for [disease]?
Background
Empowering patients, educating clinicians and aligning approaches remain critical as we work toward overcoming challenges in obtaining an accurate diagnosis for a person with a rare disease.
Unexplained symptoms, frequent hospitalizations, and misdiagnosis are common among patients living with an undiagnosed rare disease. These challenges can often also spiral into related personal, caregiver or family health issues, psychosocial, and economic burdens.
Early access to an accurate diagnosis can often lead to better prognosis, longer life expectancy, and targeted treatment plans – and help to avoid or reduce related burdens on caregivers and families. But rare disease patients – especially from underserved communities — often face unusual challenges during the diagnostic odyssey that can delay or prevent diagnosis, with tragic consequences.
For example, newborn screening has reduced the time to diagnosis and improved the prognosis for patients in more than a few rare and genetic diseases with associated treatment options. Yet, relatively little attention or support is being directed toward diseases areas where there aren’t yet approved treatments – despite the importance of screening in improving the diagnostic odyssey and helping to direct patients toward clinical trials or care options that might at least help reduce the severity or delay the onset of their conditions.
Absent access to newborn screening or other reliable testing options, patients with conditions like cystic fibrosis, sickle cell disease (SCD), betathalassemia, and spinal muscular atrophy (SMA), patients experience significantly delayed diagnoses. However, when patients are diagnosed with these conditions as newborns through government testing programs, they tend to live longer, manage their symptoms better, and have fewer emergent medical crises. Additionally, when newborn screening programs are implemented for these conditions we have an opportunity to collect near universal epidemiological data and track disease frequencies across regions and populations.
Furthermore, underserved populations with undiagnosed or under-diagnosed genetic diseases often go untreated or are under-treated and have 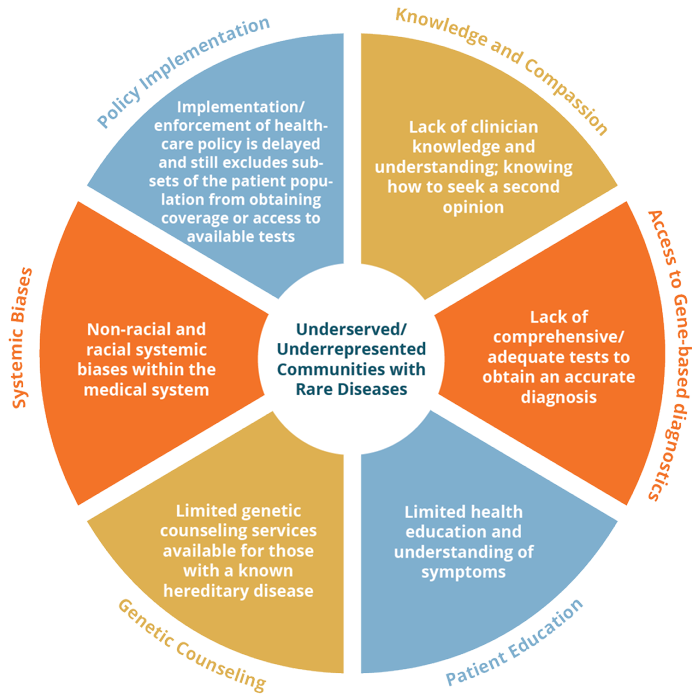 limited access to counseling or educational services about their illnesses. This global health disparity in rare disease can be overcome by increasing and advancing newborn screening methods to detect more diseases worldwide.
limited access to counseling or educational services about their illnesses. This global health disparity in rare disease can be overcome by increasing and advancing newborn screening methods to detect more diseases worldwide.
The recent addition of SMA to newborn screening programs in the United States and European Union did not sway the United Kingdom government to include this condition on its 2020 program despite requiring similar inclusion criteria, being aware of available precision therapies, and receiving pressure from patient advocacy groups.
Opportunities and Gaps
Patient advocacy organizations have helped raise medical, policy and general awareness of orphan diseases and the need to increase patient access to accurate and timely diagnoses. More must be done, however, to generate a greater sense of urgency and prioritization around underserved communities and access to screening.
Better targeted early screening methodologies hold promise for rare diseases in several disease areas examined, such as such as hereditary transthyretin (TTR) amyloidosis (hATTR) and Fabry disease. The availability of diagnostic tests and/or access to targeted therapies warrants adding these conditions to universal newborn screening programs. When confirmatory tests are available that can lead to treatment and/or better patient outcomes when implemented early in disease progression (as was noted in our review of sarcoidosis, myasthenia gravis, and primary biliary cholangitis), more must be done to increase access to such tests. Early diagnosis of acquired and late-onset rare diseases can provide medical, personal, and economic benefits, even in instances where there may not yet be an approved treatment available, and may provide opportunities for patients to be identified for clinical trials, leading to an effective treatment where none exist today.
Rare conditions with heterogeneous or misleading clinical presentation are also sometimes overlooked by physicians and specialists. Despite the availability of definitive testing strategies, varying sensitivity of those tests can limit diagnostic effectiveness with granuloma disorders like sarcoidosis. However, physiological examination, family histories, autoradiological scans, blood work, and cardiopulmonary evaluations can be powerful tools for detecting organs affected by an acquired or late-onset disease, and may indicate possible biopsy sites.
An accurate diagnosis is difficult to achieve without administering the correct test to rule out other differential diagnoses. Without medical knowledge and a high suspicion for a particular rare disease, a single physician is somewhat unlikely to accurately diagnose patients with that disease. Tools that integrate large amounts of medical information and augment clinical decision-making could help to reduce the number of overlooked and misdiagnosed patients. In some cases, data on a patient may exist in pieces across disparate medical practices and health systems but be inaccessible to a key clinician that works with a patient, or a clinical researcher looking for qualified patients for trials. In other cases, necessary data may not be available because of limitations on access to diagnostic tests or biases and hesitancies that hinder interactions with medical professionals. Irrespective of the reason, the lack of reliable access to complete patient data is another major factor that limits access to an early and reliable diagnosis.
Rare diseases with unknown causes can go undiagnosed or misdiagnosed, especially when affected patients display symptoms that mimic conditions that are relatively common in the population. In the case of narcolepsy, for example, a genetic basis is beginning to emerge, which has led to reassessment of diagnostic guidelines for this neurological disease. The onset of the condition has also been linked to prior infection with certain pathogens. Environmental exposures may also be poorly documented in the patient histories.
The range of rare disease case studies we examined demonstrated that underserved patients often face other external barriers such as geographical location and socioeconomic status, which can influence access to diagnostic testing. Despite having the medical knowledge of myasthenia gravis, for example, the physician who diagnosed Patient #8 would not have been able to do so without coordinating care internationally. Patient #8’s residence in Nepal would have otherwise prohibited her diagnosis had she not have come from affluence. The diagnostic test that ended her diagnostic odyssey was analyzed in India because it was not available in Nepal at the time. It is unknown how many people in Nepal live with this myasthenia gravis without the capacity to perform testing. In another case, Patient #7 self-diagnosed himself with Fabry’s disease using medical information on the internet, but was unconfirmed until he was tested at a center of excellence in the United States. He raised the capital necessary to relocate from South America for diagnosis and treatment, but for many patients, this option is impossible. The precision treatments for myasthenia gravis and Fabry’s disease effectively manage symptoms, but only if patients have access to an accurate and timely diagnosis.
It is important to note, however, that increased physician knowledge and patient access are unable to remedy barriers imposed by patients on their own accord, however. If patients ignore symptoms or refuse medical advice, diagnosis is nearly impossible. Patient #1 suffered with progressively worsening abdominal pain for 3+ months before seeking medical treatment for self-suspected constipation. Her condition advanced while she managed her symptoms with laxatives and acetaminophen. After extensive investigation, she was diagnosed with a rare abdominal form of sarcoidosis. Although her physicians first misdiagnosed her with a malignant abdominal cancer, causing unnecessary stress, the surgical resection of the growths within the abdomen helped to diagnose Patient #1’s condition.
A patient’s beliefs about their body, medical intervention, religion, or diseases can also limit their ability to obtain a rare disease diagnosis. Efforts to raise public awareness of rare diseases, destigmatize natural processes that cause illness, and improve quality of life for patients may help to reduce educational, ideological, and psychosocial barriers when seeking a diagnosis.
Patient mistreatment also takes many forms in the diagnostic odyssey. As a minor, Patient #5 experienced neglect when his caregivers initially dismissed his classic narcolepsy symptoms. He was also over-medicated when at least 2 specialists misdiagnosed him with psychiatric disorders and epilepsy. It is common for rare disease patients to be misdiagnosed and treated without symptom improvement. Routine monitoring of therapy responses may help alert physicians to diagnoses that should be reexamined. His condition did not improve despite medication with antipsychotics and anticonvulsive drugs, yet physicians and caregivers continued his treatment course. Because of his young age, he was unable to guide the direction of his care or diagnostic pursuits, similar to other pediatric cases. While enduring judgment by family and friends for perceived laziness, his academic life and career prospects suffered. Had he been diagnosed with narcolepsy at symptom onset, treated early with the drug that ultimately relieved his symptoms, and kept naive to psychiatric and neurological drugs, the patient could have had better medical, emotional, psychological, and socioeconomic outcomes.
Although the other case studies do not detail explicit patient mistreatment, factors internal to the patients, such as age, sex, race, ethnicity, religion, and culture can limit access to an accurate diagnosis in general. In the United States, undiagnosed cardiovascular complications in African American, Native, and Latin American women are leading causes of maternal mortality. Common explanations for this phenomenon include systemic racial bias, low adherence to follow-up visit schedules, and less than typical access to healthcare. Pregnant women, historically underserved and/or underrepresented communities, the financially unstable, and other vulnerable groups can experience preventable complications, delayed diagnosis, or misdiagnosis because of inherent characteristics that preclude them from closer examination by treating physicians.
It is well documented that physicians’ assumptions about patients based on these characteristics can hinder early diagnosis. Although patient mistreatment is not universally documented, several studies have identified diagnostic and care disparities for common physical and psychiatric diseases. In the case of Patient #9, it is unknown whether symptom oversight or sex-based microagressions contributed to his delayed diagnosis with PBC, a condition that primarily affects women. However, more work is needed to report and address potential mistreatment of patients living with the diseases that are featured in the case studies.
Although the featured cases were eventually diagnosed using the correct tests, all but Patient #10, who was screened within 12 days of birth, experienced delays to appropriate testing. A better understanding of the barriers that could have impacted their time to diagnosis could inform strategies to shorten the diagnostic odyssey. Anecdotal evidence and deliberate study of internal and external challenges in patient diagnosis is needed to supplement case studies written by treating physicians who may be unaware of or disinterested in determinants of health when reporting to the scientific community.
Just as we need unbiased tools to monitor personal health metrics (such as heart rate) and ongoing health, bias should be removed from the process of diagnosis whenever it can
cause damage to the patient. If adopted universally, these recommendations would increase diagnosis of rare and common diseases alike. A modern interpretation of rare disease statistics indicates that a high level of suspicion for a rare disease should be raised of chronic, progressive diseases that worsen or do not improve with medication until ruled out with diagnostic testing or observations.
For many in the rare disease community, diagnosis is a race against time. Future work should focus on mitigating the technical challenges associated with rare disease diagnosis (e.g. matching gene variants to disease pathology, creating multi-gene test panels targeted to symptoms, increasing accessibility to complete data sets and building diagnostic artificial intelligence, improving usability of graphical user interfaces (GUIs) by treating physicians, etc.).
Most importantly, the role of the patient advocacy organization in assembling a more complete understanding of the impact of a disease – from its diagnosis to treatment – remains central. Cultural competence in communication and service access by patient advocacy organizations serves the aims of all stakeholders, and their ability to improve trust and engagement between clinicians and patients/ caregiver.
The cycle of exclusion and disadvantage will be alleviated and disrupted by ensuring diverse patient experiences and stories are included when educating clinicians, engaging patients and caregivers, and informing the future of access. Only then will we be able to provide better outcomes and fuller lives for patients from all walks of life in the rare disease community.
Additional Global Genes Resources
Clinical Trials:
Informed Consent: Important for Treatment Decisions and Advancing Research
From Molecules to Medicine: Clinical Research
Access to Unapproved Medicine: Is This An Option for Me? (USA)
Access to Unapproved Medicine: Is This An Option for Me? (Canada)
From Molecules To Medicine: How Are New Drugs & Therapies Developed?
Diagnosis/Diagnostics:
RARE Toolkit: Genetic Testing: Is This my Path to Diagnosis?
Becoming An Empowered Patient : A Toolkit For The Undiagnosed
How to Discuss Genetic Disease with Your Loved Ones
Financial Advocacy:
Rare Insight: Building a Stronger Financial Future
Financial Advocacy in RARE: Navigating the U.S. Health System for Young Adults
Global Genes LIVE!: How to Become a Proactive Financial Advocate for Young Adults
Global Genes LIVE!: Mitigating Familial Financial Toxicity Through Planning
Taking Control: Optimizing Your Potential as a Young Adult With a Rare Disease
Healthcare Professional Programs:
Newborn Screening:
Video – Track 2: Advocacy for the Community Newborn Screening
Storytelling:
Using Storytelling To Raise Awareness For Your Rare Disease
How To Promote Your Rare Disease Story Through Social Media
Speak Easy: A Guide to Public Speaking
Download PDF
Download Now

Stay Connected
Sign up for updates straight to your inbox.
